EECP therapy in Solapur is gaining attention as a non-surgical option for managing heart blockage. This article explains how the treatment works, who may benefit from it, what to expect during sessions, and how it compares with angioplasty and bypass surgery. If you are exploring safer alternatives for heart care, this guide gives a clear overview of whether EECP could be the right choice for you or your loved one.
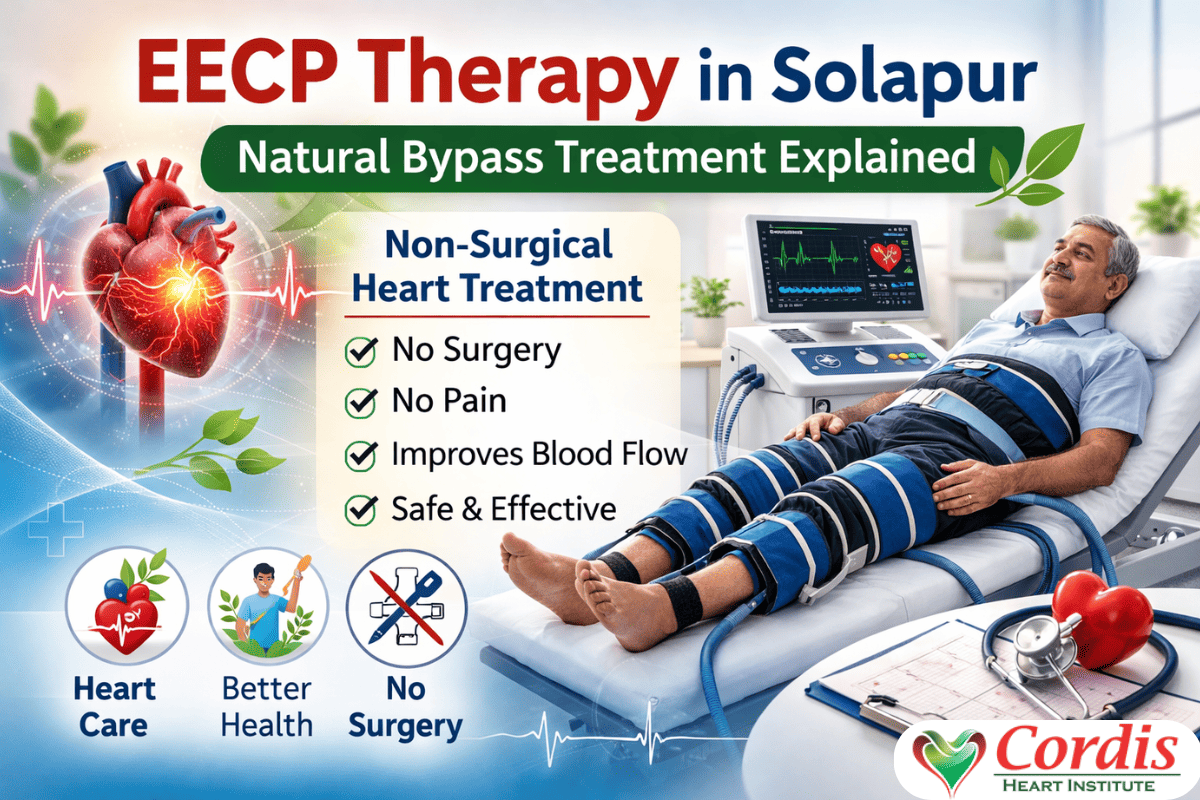
EECP Therapy in Solapur: Natural Bypass Treatment Explained
EECP therapy in Solapur is gaining attention as a non-surgical option for managing heart blockage. This article explains how the treatment works, who may benefit from it, what to expect during sessions, and how it compares with angioplasty and bypass surgery. If you are exploring safer alternatives for heart care, this guide gives a clear overview of whether EECP could be the right choice for you or your loved one.
How to Find the Best Heart Specialist Near Me for Chest Pain & Heart Blockage
Chest pain should never be ignored. Learn how to find the best heart specialist near you, recognize heart blockage symptoms, and explore modern treatment options with Cordis Heart Institute and Dr Abhijit Aklujkar.
Why Choose EECP Treatment in Mira Bhayandar for Heart Blockage?
Looking for a safe and non surgical way to treat heart blockage? EECP treatment in Mira Bhayandar is helping many patients improve heart health without surgery or long hospital stays. Learn how EECP works, its benefits, cost, and why Cordis Heart Institute with Dr Abhijit Aklujkar is a trusted choice for non invasive cardiac care.
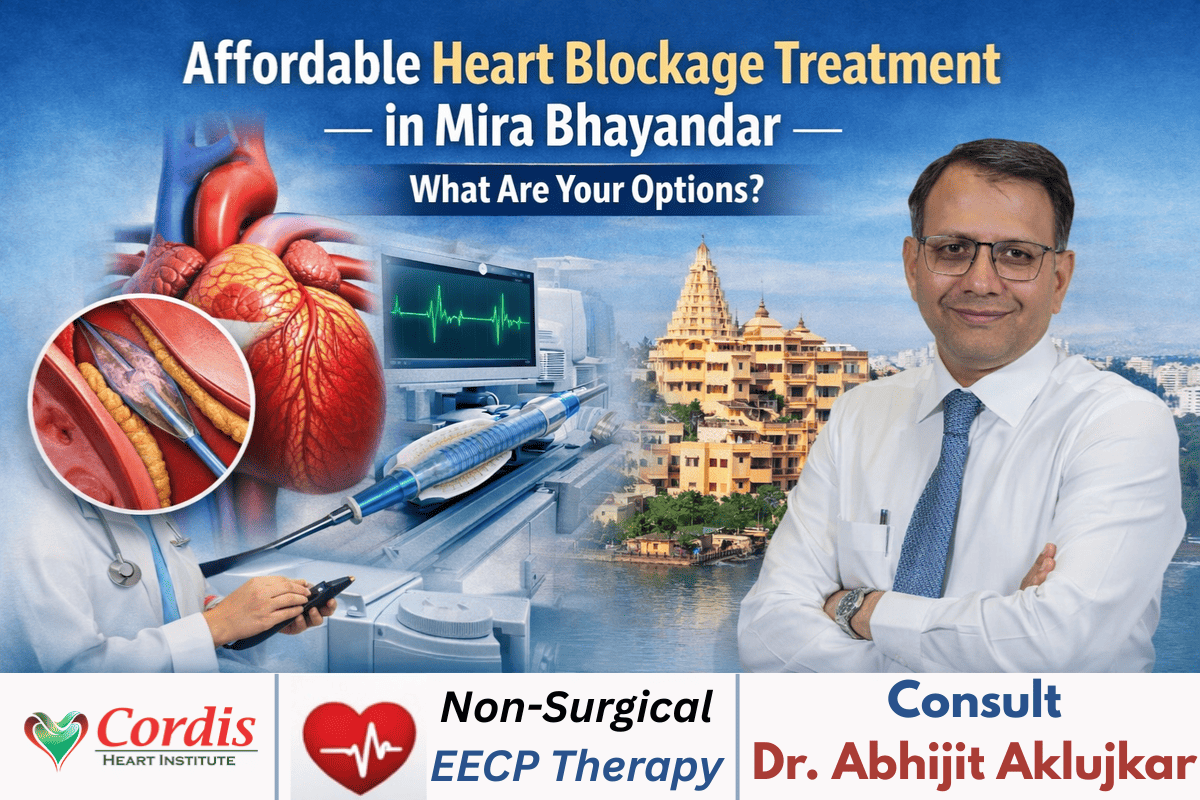
Affordable Heart Blockage Treatment in Mira Bhayandar – What Are Your Options?
Looking for affordable heart blockage treatment in Mira Bhayandar? This guide covers symptoms, test options, angioplasty, bypass surgery, and non-surgical treatments available at Cordis Heart Institute under Dr Abhijit Aklujkar.
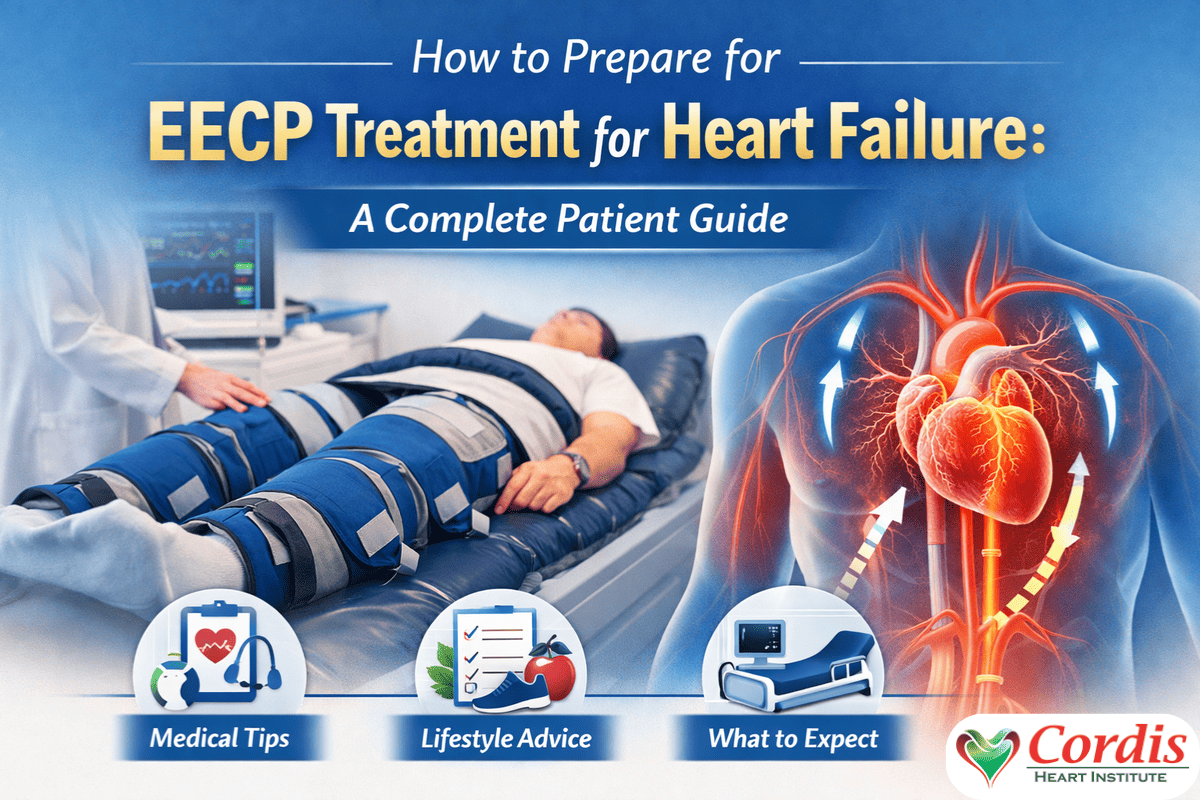
How to Prepare for EECP Treatment for Heart Failure: A Complete Patient Guide
Preparing for EECP therapy can feel overwhelming, especially if you are unsure what to expect. This guide explains how to prepare for EECP treatment for heart failure with clear, practical steps covering medical checks, lifestyle adjustments, and what happens during each session. Whether you are starting treatment soon or exploring your options, you will learn how to get ready, stay comfortable, and make the most of your EECP journey.
Cardiologists in Solapur: Complete Guide for First-Time Patients
Affordable EECP therapy offers heart patients in Solapur a safe, non-surgical alternative for controlling chest pain and enhancing blood flow. This guide shows how EECP works, what to expect in treatment, price range, and why more people are turning to eeCP as for long-term heart care with assistance from Dr. Abhijit Aklujkar.
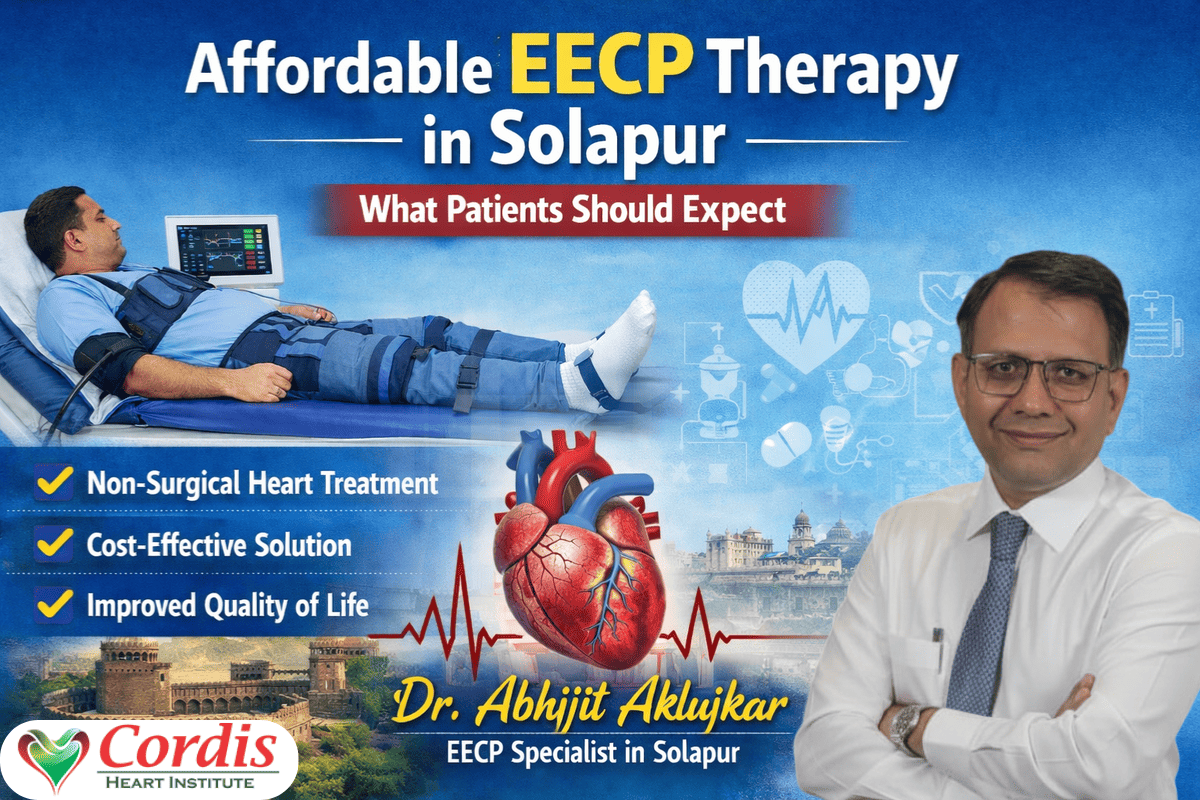
Affordable EECP Therapy in Solapur: What Patients Should Expect
Affordable EECP therapy offers heart patients in Solapur a safe, non-surgical alternative for controlling chest pain and enhancing blood flow. This guide shows how EECP works, what to expect in treatment, price range, and why more people are turning to eeCP as for long-term heart care with assistance from Dr. Abhijit Aklujkar.
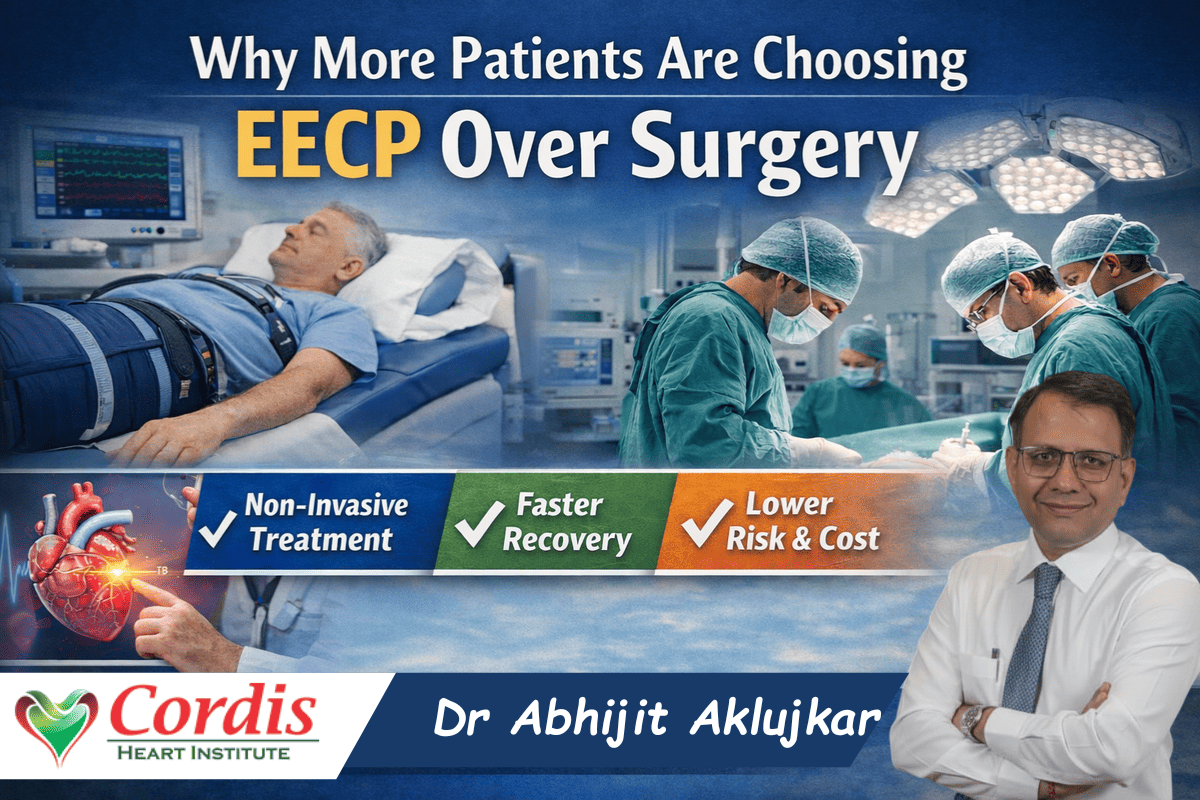
Why More Patients Are Choosing EECP Over Surgery
Patients looking for safer alternatives to heart surgery are increasingly turning to EECP therapy. This article explains why EECP over surgery is gaining popularity, how it improves heart circulation without invasive procedures, and the key benefits for long term heart health. Learn how expert care at Cordis Heart Institute with Dr Abhijit Aklujkar helps patients choose effective non surgical treatment options for a better quality of life.
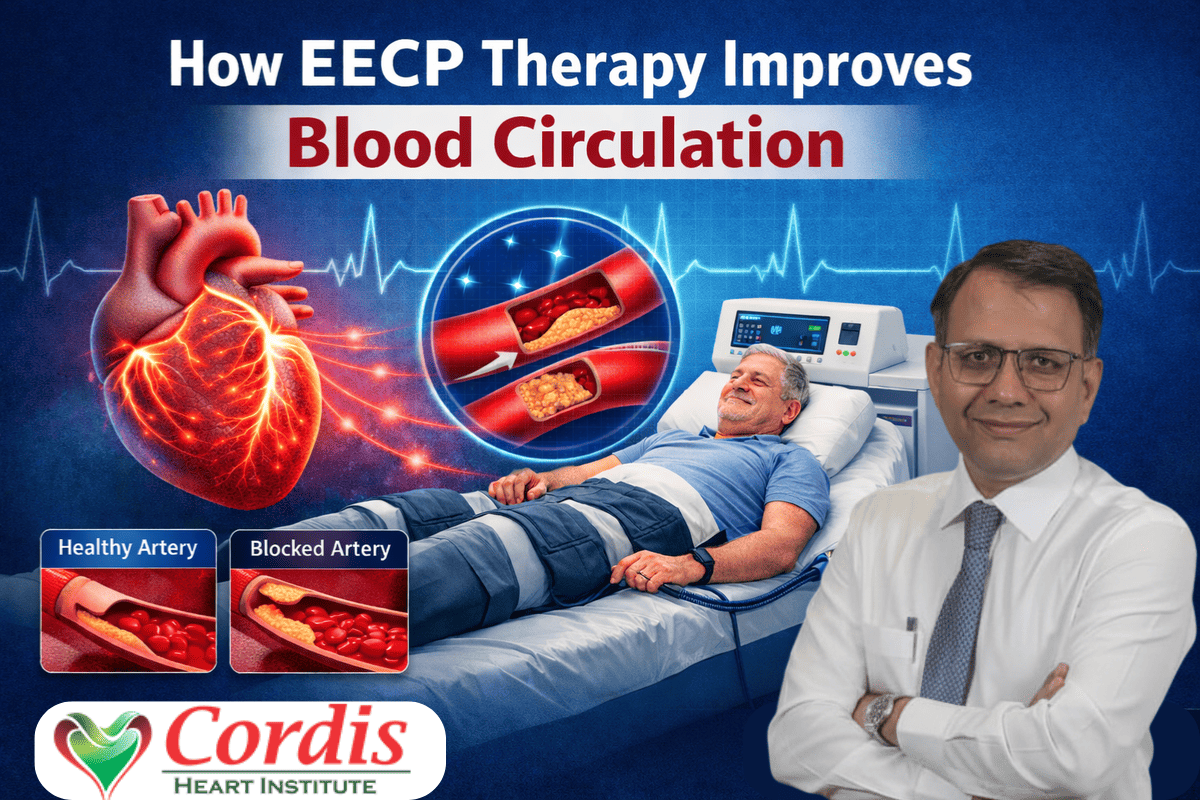
How EECP Therapy Improves Blood Circulation
EECP therapy is a non surgical heart treatment that helps improve blood circulation and support better heart function. This guide explains how EECP therapy works, its benefits for patients with chest pain or blocked arteries, and what to expect during treatment at Cordis Heart Institute with Dr Abhijit Aklujkar. Learn how this safe and clinically proven therapy can help increase blood flow to the heart and improve quality of life.