Excess weight can increase blood pressure and raise the risk of heart disease. This article explains how obesity treatment in Mira Bhayandar helps control hypertension through medical weight management, lifestyle changes, and expert cardiac care at Cordis Heart Institute.
How Obesity Treatment in Mira Bhayandar Helps Reduce Blood Pressure
Excess weight can increase blood pressure and raise the risk of heart disease. This article explains how obesity treatment in Mira Bhayandar helps control hypertension through medical weight management, lifestyle changes, and expert cardiac care at Cordis Heart Institute.
Heart Hospital Mumbai: How to Choose the Right Cardiac Hospital for Treatment
Looking for the right heart hospital in Mumbai can feel overwhelming, especially when your health is at stake. This guide breaks down exactly what to look for in a cardiac hospital, from experienced cardiologists and advanced treatment options to ICU facilities and emergency care. Discover how Cordis Heart Institute and Dr Abhijit Aklujkar provide focused, patient-centered cardiac treatment in Mumbai, helping you make a confident and informed decision for your heart health.
EECP Therapy in Mumbai: Which Cardiologists Offer It?
EECP therapy is a non-surgical heart treatment helping patients in Mumbai improve blood flow, reduce chest pain, and avoid surgery. This guide explains how it works, its cost, benefits, and where to get treated at Cordis Heart Institute with Dr Abhijit Akuljkar.
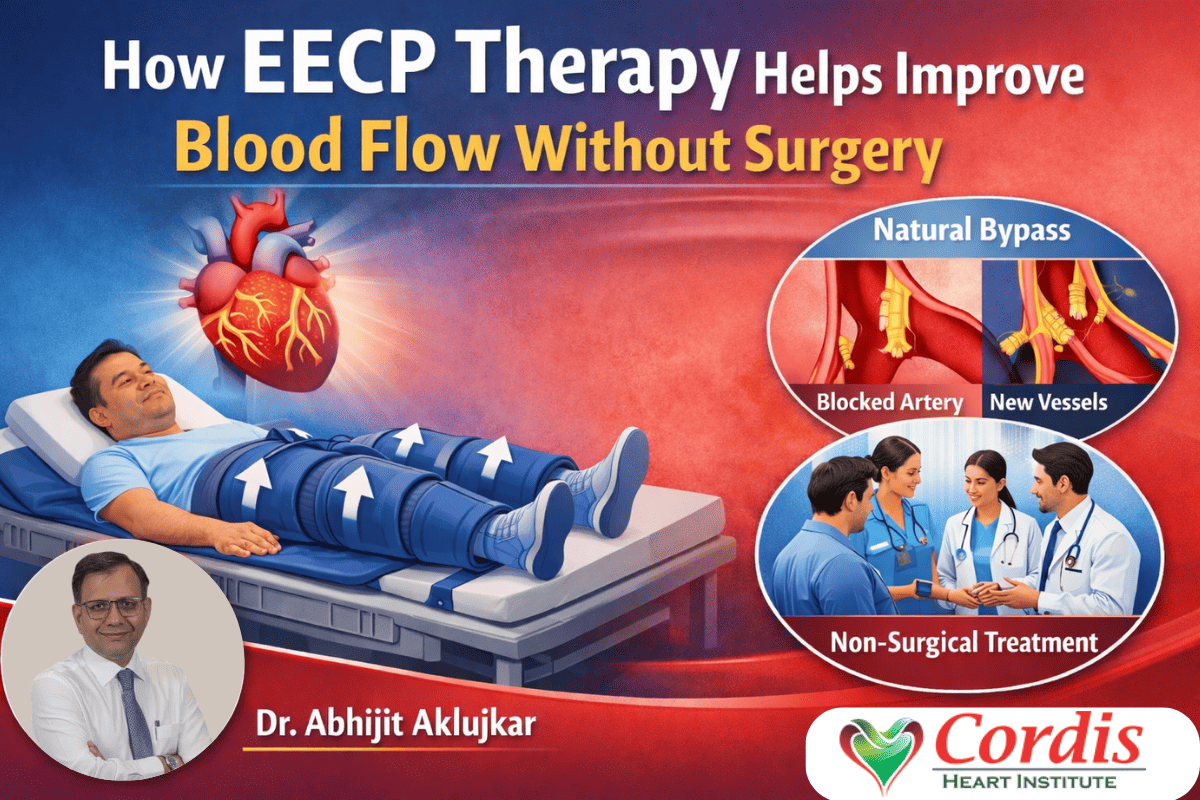
How EECP Therapy Helps Improve Blood Flow Without Surgery
EECP therapy is a non-surgical heart treatment that helps improve blood flow and reduce chest pain by encouraging the body to develop natural bypass vessels. This guide explains how the therapy works, who can benefit from it, what happens during treatment, and why many patients choose it as an alternative to angioplasty or bypass surgery at Cordis Heart Institute under Dr Abhijit Aklujkar.
Top Signs You Should Visit an Obesity Clinic in Mira Road
Struggling to lose weight despite dieting and exercise? This blog explains the key warning signs that indicate it may be time to visit an Obesity Clinic in Mira Road. Learn how medical weight loss at Cordis Heart Institute can help you manage weight safely, prevent lifestyle diseases, and achieve long-term health results.
Best Obesity Treatment Doctors in Mumbai: How to Choose the Right Specialist
Choosing the best obesity treatment doctors in Mumbai can make all the difference when diet and exercise alone are not enough. This guide explains how to pick the right specialist, explore treatment options, and start a safe, medically guided weight loss journey with Cordis Heart Institute.
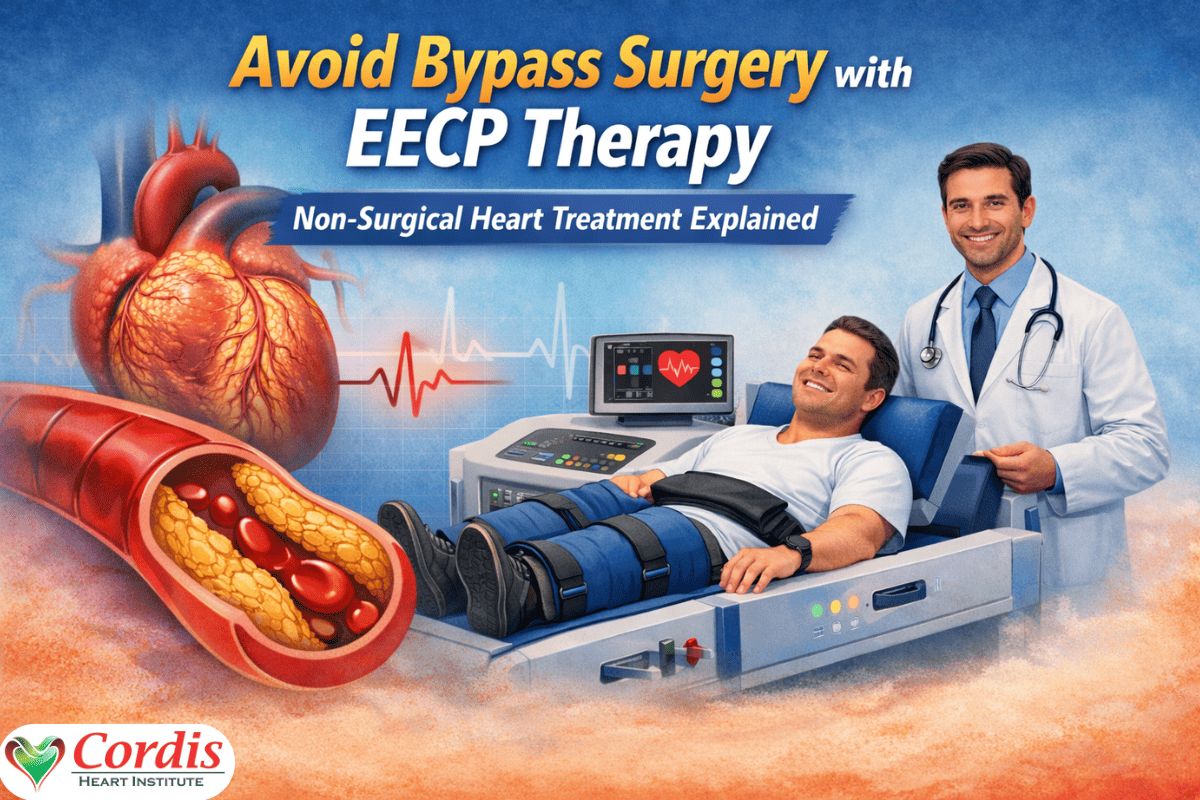
Avoid Bypass Surgery with EECP Therapy: Non-Surgical Heart Treatment Explained
Many heart patients are advised bypass surgery without knowing that a non-invasive option may be available. This article explains how EECP therapy improves blood circulation, reduces chest pain, and supports heart health without surgery. Learn who can benefit, how the treatment works, and what to expect from EECP therapy at Cordis Heart Institute with Dr Abhijit Aklujkar.
How to Choose the Best Cardiologist in Mulund: A Complete Patient Guide
A simple guide to choosing the best cardiologist in Mulund, when to see a heart specialist, and why Cordis Heart Institute with Dr Abhijit Aklujkar is trusted for heart care.
Heart Blockage Treatment Without Surgery in Thane: All Available Options
Many people believe surgery is the only solution for heart blockage, but modern cardiology offers effective non-surgical treatments that can improve blood flow and reduce symptoms. This article explains all available heart blockage treatment options without surgery in Thane, including EECP therapy, lifestyle changes, medications, and who can benefit from these treatments at Cordis Heart Institute under Dr Abhijit Aklujkar.